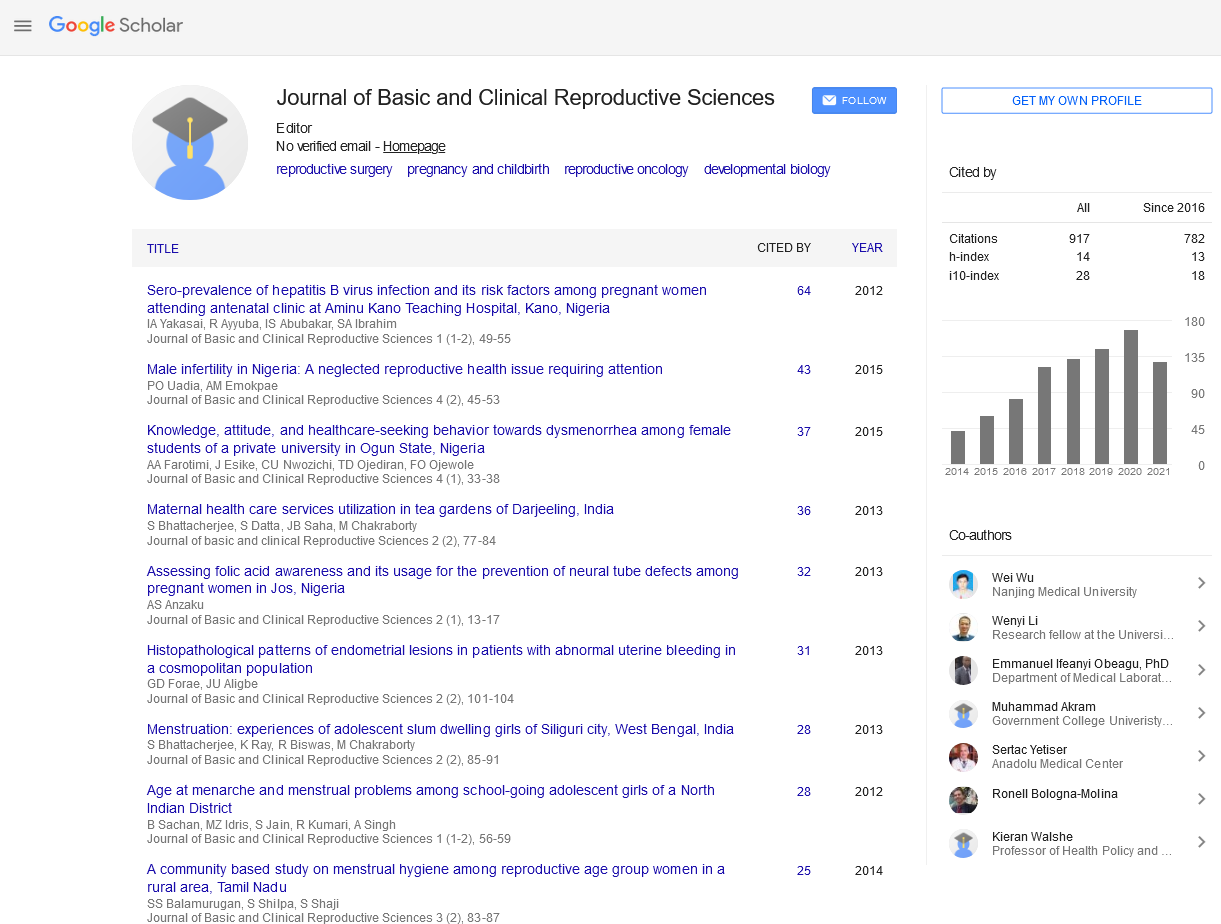
Research Article - Journal of Basic and Clinical Reproductive Sciences (2017) Volume 6, Issue 2
Uptake and Predictors of Long-Acting Reversible Contraceptives among Women in a Tertiary Health Facility in Northern Nigeria
Received: 10-May-2017 Accepted Date: Aug 24, 2017 ; Published: 20-Sep-2017
Citation: Mohammed D.A,Joel A,Bature S,Abubakar A,Mohammed C,Taingson M.Uptake and Predictors of Long-Acting Reversible Contraceptives among Women in a Tertiary Health Facility in Northern Nigeria doi: 10.4103/2278-960X.194504
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Introduction
Nigeria has a total fertility rate of 5.5 births, and this is higher in the North-west zone with 6.7 births [1]. Unfortunately, this is accompanied by a high maternal mortality ratio of 560:1. Contraception is one of the strategies that can be used to significantly reduce maternal mortality [2].
While knowledge of contraception is generally high in Nigeria, contraceptive uptake is still low. About 85 percent of Nigerian women and 95 percent of men report knowing about at least one contraceptive method, yet only ten percent of currently married women report using a modern contraceptive method. The median birth interval in Nigeria is 31.7 months [1], so LARC (long acting reversible contraceptives) would be an ideal choice for Nigerians. Typically, LARC refers to intrauterine devices IUD (effective for 5-10 years) and implants (effective for up to 3 years). However, the most commonly used modern contraceptive methods in Nigeria are short acting reversible contraceptives (SARC); Injectables (3 percent), male condoms (2 percent), and the pill (2 percent) are 1. Knowledge of IUD is 31.8% and of implant is 24.7% [1]. Uptake of LARC is low; the use of IUD increased slightly from 0.8% in 1990 to 1.1 in 2013 [1].
The use of LARC methods offers a lot of advantages. They are very effective [3]. Their effectiveness is independent of user age or compliance and is more than most other forms of contraception; the unintended pregnancy rate within a year of typical use for oral contraception, hormonal patch, rings, injectables, intrauterine devices, levonorgestrel intrauterine device, subdermal implant and sterilisation are 9%, 9%,9%, 6%, 0.8, 0.2, <0.1 and <0.5 respectively [4,5]. Unlike sterilization, LARC has no requirement for surgery [6,7]. They also generally require little intervention on the part of the user and do not interfere with sex, are very cost-effective allaying high upfront costs through long-term benefits, have limited contraindications for use, can be inserted right after delivery or abortion and fertility is rapidly restored following removal [3,7,8]. Offering LARC after 1st trimester abortion leads to a greater reduction repeat abortions than with other forms of contraception [9]. Design improvements have improved their side effect profile, improved patient acceptability and made insertion/removal simpler [3]. However, the effectiveness of the devices such as IUD remains dependent on proper insertion technique, which varies in complexity by individual device [7]. Expulsion of IUDs is reported in 1 in 20 women, with a higher frequency observed within the first 3 months after insertion and during menstruation [7].
Despite barriers and myths among health care providers, LARC has been found to be easy to insert and is well tolerated among nulliparous women, and does not increase the risk for pelvic inflammatory diseases (PID) [10].
Despite the benefits of LARC methods they continue to be used less frequently than user-dependent methods in many regions [6,7,11]. LARC methods may be underused for several reasons, including misperceptions and misinformation about them, higher initial cost, ‘provider dependence’ and requirements for specific clinical skill, and provider bias against the method [7]. Thus, a lack of education and training by health care professionals may result in significant barriers to LARC access [3,12], though counselling increases LARC use as shown in the United States Contraceptive CHOICE project [13].
The objective of this study was to determine the uptake and predictors of long-acting reversible contraceptives among women in our setting so that strategies can be put in place to maximise their benefits.
Materials and Methods
The study setting was a tertiary hospital located in Kaduna, northern Nigeria and catering for the metropolis and its environs. Approval for the study was gotten from the Kaduna state ministry of health. There was no risk to clients whose information was kept confidential. We used a retrospective study design to evaluate uptake of LARC (intrauterine contraceptive devises and implant). All available client records from the family planning clinic from January 1st, 2000 to March 31st, 2014 were retrieved. Information was collected on demographics, reproductive, menstrual and contraceptive history and method of contraception chosen at the first visit. Data was analyzed using the statistical package for social sciences (SPSS) version 15. Missing responses were stated as such and excluded from analysis. Descriptive analysis was done using frequencies and percentages. Chi square was used as a test of association between method of contraception and demographic/other relevant factors such as reason for contraception and previous use. Significance level established at P value of 0.05.
Results
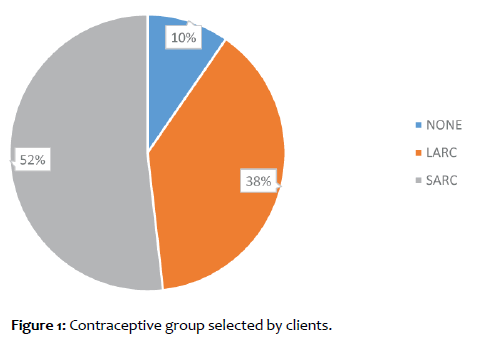
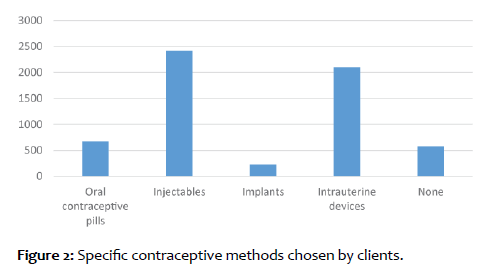
A total of 5992 family planning record cards were retrieved. Some 2319 clients selected to use LARC (38.7%), while 3096 used SARC (51.7%) and 577 did not select a method at the first visit (9.6%) (Figures 1 and 2).
Intrauterine devices were the chosen LARC for 2047clients (90.2%) and all were copper T brands, while 223 clients (9.8%) used contraceptive implants (Implanon and Jadelle brands). The SARC used were oral contraceptive pills and injectables. There were no records for barrier methods or permanent forms of contraception.
Clients using LARC were mostly aged 25 to 39 years, educated up to secondary level or more, Muslims, source of information was mainly from clinic personnel and friends/relatives, had at least one living child and less miscarriages, still wanted more children (“spacers”) and previous contraception used was also LARC (all intrauterine devices and no implants). When LARC was compared to SARC, all demographic and other characteristics of clients as shown in Table 1, were had significantly different (p value <0.05). Those that are not very educated are more likely to use SARC, while the more educated were more likely to use LARC. Those aged 45 years and above were more likely to use LARC, while those <20 years were more likely to use SARC. Those using LARC were less likely to get information from television. Those with fewer numbers of living children were more likely to use LARC while those with more children were more likely to use SARC. Those with fewer numbers of miscarriages/stillbirths were more likely to use LARC while those with more miscarriages/stillbirths were more likely to use SARC. Those who wanted more children were less likely to use LARC. Clients were more likely to continue the same contraceptive group as their previous contraceptive method, with those choosing LARC most likely to have used intrauterine devices in the past.
| Characteristic | SARC | LARC |
|---|---|---|
| Age (n=5414) | ||
| <20 | 106 | 15 |
| 20-24 | 613 | 293 |
| 25-29 | 803 | 522 |
| 30-34 | 820 | 733 |
| 35-39 | 499 | 422 |
| 40-44 | 184 | 233 |
| 45-49 | 29 | 101 |
| =50 | 41 | 0 |
| X=232.533 | ||
| df=7 | ||
| p=0.000 | ||
| Education (n=5387) | ||
| None | 370 | 155 |
| Some primary | 218 | 120 |
| Completed primary | 444 | 183 |
| Some secondary | 455 | 175 |
| Completed secondary or more | 1609 | 1658 |
| X=235.246 | ||
| df=4 | ||
| p=0.000 | ||
| Religion (n=5328) | ||
| Islam | 1900 | 1181 |
| Christianity | 1122 | 1092 |
| Others | 23 | 10 |
| X=65.681 | ||
| df=2 | ||
| p=0.000 | ||
| Source of information (n=5378) | ||
| Clinic personnel | 2132 | 1523 |
| Outreach personnel | 27 | 26 |
| Radio | 146 | 92 |
| TV | 107 | 70 |
| Print media | 18 | 0 |
| Friend/relative | 604 | 578 |
| Another clinic | 2 | 12 |
| Community health worker | 33 | 2 |
| other | 0 | 6 |
| X=74.742 | ||
| df=8 | ||
| p=0.000 | ||
| Number of living children (n=5328) | ||
| 0 | 0 | 0 |
| 01-Feb | 979 | 777 |
| 02-Apr | 839 | 793 |
| =4 | 1200 | 740 |
| X=40.235 | ||
| df=2 | ||
| p=0.000 | ||
| Number of miscarriages or Stillbirths (n=1524) | ||
| 0 | 499 | 515 |
| 01-Mar | 224 | 63 |
| >3 | 105 | 118 |
| X=80.498 | ||
| df=2 | ||
| p=0.000 | ||
| Want more children? (n=5325) | ||
| No | 393 | 215 |
| Yes | 2503 | 1916 |
| Unsure/undecided | 134 | 164 |
| X=32.271 | ||
| df=2 | ||
| p=0.000 | ||
| Type of previous contraception (n=2418) | ||
| None | 29 | 1 |
| Oral contraceptive pills | 427 | 226 |
| Injectables | 604 | 475 |
| Intrauterine devices | 174 | 482 |
| X=247.107 | ||
| df=3 | ||
| p=0.000 | ||
n=number of clients, X=chi square, df=degree of freedom, p=p value
Table 1: A comparison of characteristics of clients choosing SARC (short acting reversible contraception) and LARC (long acting reversible contraception).
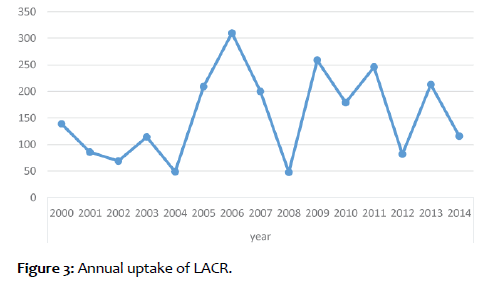
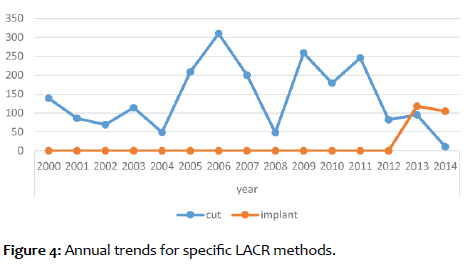
Figure 3 show the annual trends in LARC uptake with a peak in 2006. As shown in figure 4, the use of IUD peaked in 2006 and has been on a slow decline. Contraceptive implants were not used in the study facility till 2012 and its use has been on a steady increase.
Discussion
The proportion of women using a long-acting reversible contraceptive (LARC) method-IUD, implants, or injectables-has increased in low-income countries over the past few decades [14,15]. The 38.7% uptake of LARC found in this study is high when compared to that of the 2013 Nigerian health and demographic survey; only IUD was mentioned and its use was low but increased slightly from 0.8% in 1990 to 1.1 in 2013 [1]. In Zambia, LARC use was reported by less than 1% of respondents in 2004 but had increased to 9% by 2011 [16]. Data for the mid-to-late 2000s indicate that LARC was used by 15% of contraceptors worldwide, including 11% of British users, 23% of French users, 27% of Norwegian users, and 41% of Chinese users [3]. The US rates of LARC then were much lower than our Europe because sterilization is more common in the United States [3]. An analysis of a cohort of 9,256 women in the Contraceptive CHOICE project showed more than 75% chose an IUD or implant as their contraceptive method and a reduction in abortion rates, repeat abortions and teenaged birth rates [13] highlighting the increasing uptake of LARC and its benefits.
Non-hormonal IUD was most commonly used (all Copper T brands) and this is commonly associated with menorrhagia which may impede uptake. Though hormonal IUD significantly reduces menorrhagia (such as the Mirena brand by Bayer with levonorgestrel), it was not available in the study facility. Mirena is not widely available in Nigeria and is expensive, but cheaper unbranded forms are available in only few centres. The types and brands of contraceptives (including LARC), as well as knowledge and training of service providers available in most Nigerian centres has a narrow scope, and is probably heavily dependent on available supply and interests of non-governmental partners supporting government in such facilities.
Clients aged 45 years and above were more likely to use LARC, while those <20 years were more likely to use SARC. Perhaps those above 45 have already attained good family size and want LARC to carry them into menopause. So, it is not surprising that those desiring more children were less likely to use LARC. Women who had experienced one or two live births, and particularly those under 30 years, saw some of the largest increases in LARC use in 2009 in the US, which may indicate a provider-level bias for LARC methods toward women who have already reached their fertility intentions [3]. In Zambia, Factors associated with LARC use included having at least ones child 16. Younger nulliparous women were less likely to have LARC removed early [17]. Yet age and nulliparity are not contraindications to use of LARC by adolescents [18].
Clients using LARC were mostly educated up to secondary level or more, the more educated were more likely to use LARC. This is common to all contraceptives probably because of increased awareness and understanding. In Zambia, women with less education were less likely to report LARC use [16].
Clients were more likely to continue the same contraceptive group as their previous contraceptive method, with those choosing LARC most likely to have used intrauterine devices in the past. This is probably because they are already used to the method, are satisfied with it and have adapted to its side effects if any. One study showed high satisfaction rates with LARC [17].
Annual trends in LARC uptake in the study setting showed slow decline in IUD and increase in contraceptive implants. This was like a study in Ibadan that showed demand for IUD did not show an upward trend over time but increased greatly years after the free access to contraception. Similarly demand for implant at the health facility has kept growing with time [19]. The nonuse of implants before 2012 and increase thereafter reinforces the notion that service provider training (and thus bias) and supply by supporting non-governmental organization may affect contraceptive trends in different area of the country. Data for current contraception in our study was taken at the first visit, while one American study showed that the vast majority of obstetrician gynecologists offer IUDs (95.8 %), but a majority require two or more visits, which is a potential barrier to more wide spread use [20,21].
Conclusion
Uptake of LARC is encouraging but still underutilised in the study setting, especially by young nulliparous women. Contraceptive counselling of women should be improved to emphasise the high efficacy, safety and relatively few contraindications of LARC and dispel myths. Uniform country wide training of service providers and consistent supply of LARC should be ensured by government. A wider scope of LARC (hormonal IUD) needs to be made available and affordable to Nigerian women. Girl child education should be continued and expanded for its positive impact on contraceptive uptake.
Disclosure
Authors have no financial disclosures or conflicts of interest to declare.
REFERENCES
- National Population Commission (NPC) [Nigeria] and ICF International. Demographic and Health Survey 2013. Abuja, Nigeria, and Rockville, Maryland, USA.
- Ahmed S, Li Q, Liu L, Tsui AO. Maternal deaths averted by contraceptive use: an analysis of 172 countries. The Lancet, 2012.
- Finer LB, Jerman J, Kavanaugh ML. Changes in use of long-acting contraceptive methods in the U.S. 2007–2009. 2012;98:893-897.
- Trussel J. Contraceptive failure in the United States. Contraception 2011;83;397-404.
- Winner B, Peipert JF, Zhao Q, Buckel C, Madden T, Allsworth J, et al. Effectiveness of longacting reversible contraception. N Engl J Med 2012;366:1998–2007.
- Trussell J, Wynn LL . Reducing unintended pregnancy in the United States. Contraception 2008;77:1-5.
- Blumenthal PD, Voedisch A, Gemzell-Danielsson K. “Strategies to prevent unintended pregnancy: increasing use of long acting reversible contraception.†Human Reproduction Update 2011;17:121-137.
- Trussell J, Lalla AM, Doan QV, Reyes E, Pinto L, Gricar J. Cost-effectiveness of contraceptives in the United States. Contraception 2009;79:5-14.
- Rose SB, Lawton BA. Impact of long-acting reversible contraception on return for repeat abortion.Am J Obstet Gynecol. PLoS One 2012;7:e48948
- Buhling KJ, Hauck B, Dermout S, Ardaens K, Marions L. Understanding the barriers and myths limiting the use of intrauterine contraception in nulliparous women: results of a survey of European/Canadian healthcare providers. Eur J Obstet Gynecol Reprod Biol 2014;183:146–154
- D’Arcangues C. Worldwide use of intrauterine devices for contraception. Contraception 2007;75:S2–7.
- Rafie S, McIntosh J, Shealy KM, Borgelt LM, Forinach A, Shrader SP, et al. PRN Opinion Paper: Roles of the pharmacist in the use of safe and highly effective long-acting reversible contraception: An opinion of the Women’s Health Practice and Research Network of the American College of Clinical Pharmacy. Pharmacotherapy 2014;34:991–999.
- Peipert JF, Madden T, Allsworth JE, Secura GM. Preventing unintended pregnancies by providing no-cost contraception. Obstet Gynecol 2012;120:1291-1297.
- Bertrand JT, Sullivan TM, Knowles EA, Zeeshan MF, Shelton JD. “Contraceptive Method Skew and Shifts in Method Mix in Low-and Middle-Income Countries.†International Perspectives on Sexual and Reproductive Health 2014;40:144-153.
- Staveteig S, Mallick L, Winter R. Uptake and Discontinuation of LongActing Reversible Contraceptives (LARCs) in Low-Income Countries. DHS Analytical Studies No. 54. Rockville, Maryland, USA: ICF International 2015.
- Hancock NL, Chibwesha CJ, Stoner MCD, Vwalika B, Rathod SD, et al. Temporal Trends and Predictors of Modern Contraceptive Use in Lusaka, Zambia, 2004–2011. Biomed Res Int 2015;2015:521928.
- Dickerson LM, Diaz VA, Jordan J, Davis E, Chirina S, et al. Satisfaction, Early Removal, and Side Effects Associated with Long Acting Reversible Contraception. Fam Med 2013;45:701-707.
- ACOG- Adolescents and long-acting reversible contraception: implants and intrauterine devices. Committee Opinion No. 539. American College of Obstetricians and Gynecologists. Obstet Gynecol 2012;120:983–988.
- Adako O, Okunfulure FO. Demand for Long Acting Reversible Contraceptives and Associated Factors among Women Accessing Family Planning Service in ARFH Model Clinic Ibadan, South West Nigeria. Adv Practice Nurs. 2016;1:117.
- Luchowski AT, Anderson BL, Power ML, Raglan GB, Espey E, Schulkin J. Obstetician-Gynecologists and contraception: long-acting reversible contraception practices and education. Contraception. 2014;89:578–583.
- Shoupe D. LARC methods: entering a new age of contraception and reproductive health. Contraception and Reproductive Medicine 20161:4.