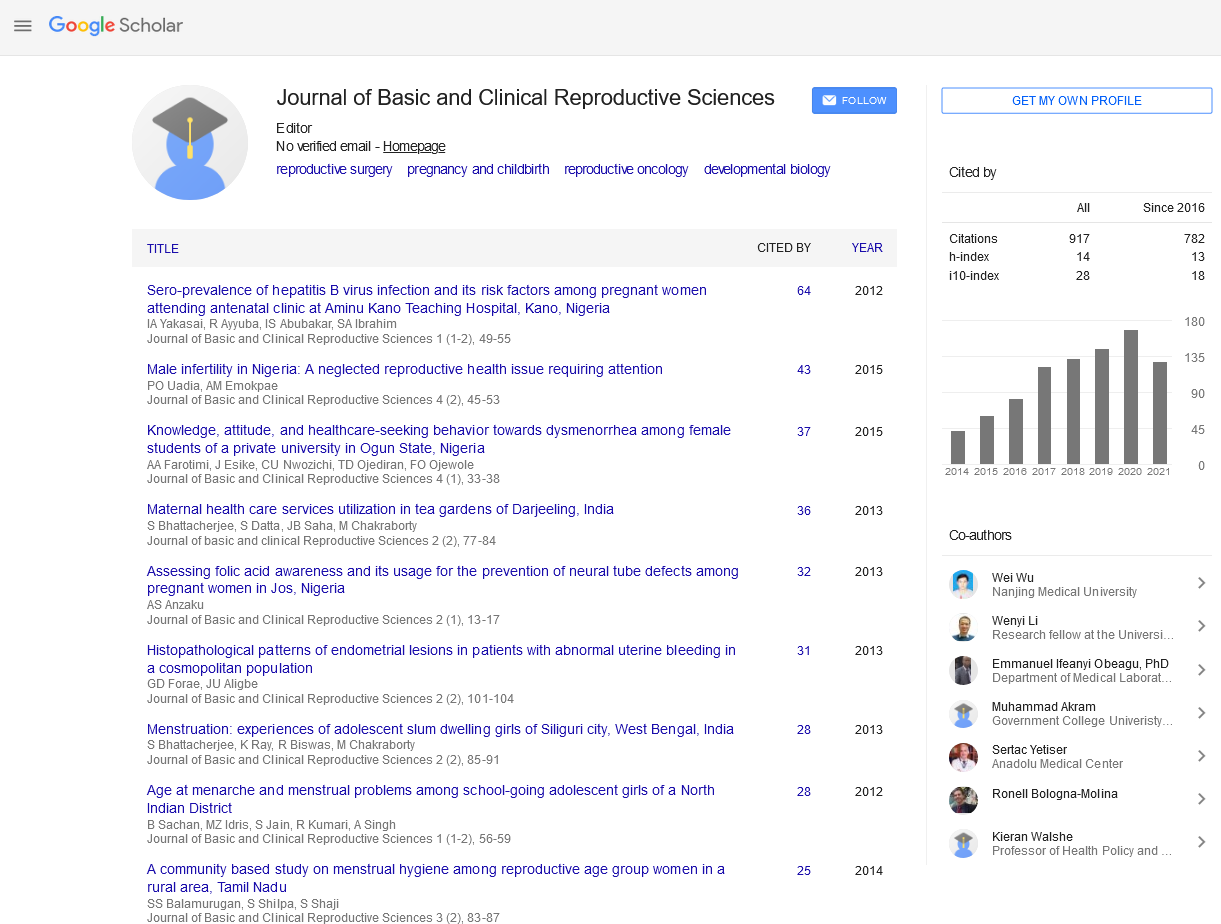
Original Article - Journal of Basic and Clinical Reproductive Sciences (2017) Volume 6, Issue 2
Gender Based Changes in Cord Blood Heme Oxygenase-1
Received: 30-May-2017 Accepted Date: Dec 02, 2017 ; Published: 12-Dec-2017
Citation: Kharb S.Gender Based Changes in Cord Blood Heme Oxygenase-1 doi: 10.4103/2278-960X.194506
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Evidences support the role for the heme oxygenase system (HO-1) in the maintenance of a healthy pregnancy, especially during pathological challenge. To study gender-based changes in HO-1 levels in cord blood by comparing the concentrations of heme oxygenase-1 in maternal and cord blood venous sample of normotensive pregnant and preeclamptic women. Fifty pregnant women were selected and grouped as group 1 (control, n=25) comprising of normotensive women immediately after delivery; Group 2 (study group, n=25) comprising of age-and sex-matched preeclamptic women. Study samples were drawn (maternal venous blood and umbilical cord blood) and heme oxygenase-1 was analyzed by competitive enzyme linked immunosorbent assay. There was significant rise in serum heme oxygenase 1 levels in preeclamptic women as compared to normotensive pregnant women (p<0.001). Cord blood hemeoxygenase-1 levels in preeclamptic women were also significantly higher than normotensive counterpart (p<0.001).The cord blood heme oxygenase-1 levels in both the groups were comparable with their maternal levels. Maternal HO-1 were higher in mothers with female babies as compared to male (285.30 ± 28.40 ng/ml vs. 268.41 ± 35.00 ng/ml, p>0.05) in group I. Maternal HO-1 were higher in preeclamptic mothers with female babies as compared to male counter parts in group II (580 ± 111.28 ng/ml vs. 526.2 ± 74.3 ng/ml, p>0.05 ). Cord blood HO-1 were higher in female babies as compared to male babies in group I (279.23 ± 30.9 5 ng/ml vs. 273.75 ± 33.45 ng/ml, p>0.05). Cord blood HO-1 were higher in females as compared to male in group II (560.83 ± 67.33 ng/ml vs. 534.89 ± 63.76 ng/ml, p>0.05). Demonstration of gender based changes in the present study supports the idea of active contribution of placenta to maternal metabolism during pregnancy.
Keywords
Heme oxygenase, Gestational age, Pregnancy, Preeclamptics, Cord blood.
Introduction
Preeclampsia is a multi-system disorder of pregnancy [1]. The basic pathology of preeclampsia is intense vasospasm affecting the vascular system, especially renal, uterine and cerebral vessels. The cause of this vasospasm is probably due to an increase in vasopressor substances like angiotensin II, thromboxane A2, endothelin I and a decrease in vasodilator substances such as nitric oxide and prostacyclin due to endothelial cell dysfunction [2].
Heme oxygenase (HO) is a rate-limiting enzyme in heme production. HO enzyme consists of two isoform, HO-1 and HO-2 and each break down heme to biliverdin, carbon monoxide (CO) and free iron. HO-1 is cytoprotective and exerts anti-inflammatory effects and regulates cell proliferation. HO-1 plays a central role in the pathogenesis of immune mediated inflammatory diseases [3]. In mice, HO-1 is expressed in the ovaries and deficiency of HO-1 in them causes deficient ovulation [4].
A role for HO-1 in pregnancy has been suggested and it has been reported to be synthesized within the fetoplacental unit. HO-1 is an endogenous system that offers protection against cytotoxic damage in the placenta, identifies the HO-CO (heme oxygenase- carbon monoxide) pathway to regulate fetoplacental circulation [5]. Up on fecundation, HO-1 is seen very early in pregnancy. In blastocyst stage, its presence indicates attachment ability of blastocyst with uterine epithelial cells and hence implantation occurs. Absence of HO-1 implies a deficient or absence of implantation [6]. HO-1 facilitates implantation of fertilized blastocyst and this is mediated by its metabolite CO, which prevents accumulation of free heme. The on-time implantation in the presence of HO-1 is followed by a normal implantation, fetal growth and wellbeing. In the absence of HO-1, excess free heme causes cell damage and finally leads to aberrant implantation, IUGR and /or fetal loss [7].
There is still no evidence regarding umbilical cord HO-1 levels in preeclampsia. The extent to which HO-1 per se mediates the fetal growth and developmental abnormalities associated with disease states such as diabetes, hypoxia, or preeclampsia remains to be fully clarified. No data are available on the possible association of fetal growth with levels of HO-1.
Since cord blood can serve as diagnostic window for future risk of cardiovascular disease in both mother and new-born. The present study was planned to study both maternal as well as fetal aspects of preeclampsia by comparing HO-1 levels in maternal and umbilical cord venous samples. Also, it was planned to assess the gender-based changes in HO-1 levels in cord blood by comparing the concentrations of heme oxygenase-1 in maternal and cord blood venous sample of normotensive pregnant and preeclamptic women.
Materials and Methods
The present study was conducted during 2015-2016 in the Department of Biochemistry in collaboration with Department of Obstetrics and Gynaecology. This study was approved by Ethics Review Committee of the Institute. Fifty pregnant women attending the Outpatient Department of Obstetrics and Gynaecology were randomly enrolled in the study and divided into two groups namely, group I (control, n=25) comprising normotensive women with singleton pregnancy immediately after delivery and group II (study, n=25) included gestation- matched women with singleton pregnancy and systolic blood pressure reading 140 mmHg or diastolic blood pressure 90 mmHg with or without proteinuria immediately after delivery [1]. Informed consent was taken from all the patients. Women with a history of chronic hypertension, any metabolic disorder before or during pregnancy, or presence of high risk factors like anemia, heart disease, diabetes, liver disease, renal disease were excluded from the study. Five millilitres of maternal venous blood sample was collected aseptically from antecubital vein and 10 ml of cord blood was collected from placental end of umbilical cord at the time of delivery. The serum was separated by centrifugation and analyzed the same day.
Routine investigations and serum HO-1 levels were analyzed in maternal and cord blood of preeclampsia and normotensive pregnant women. HO-1 levels in serum were analyzed by using double-antibody sandwich enzyme- linked immunosorbent assay kits (QAYEE-BIO) [8].
Results were expressed as mean values+Standard deviation and student’s ‘t’ test was applied. Data were considered to be significant if p<0.05 and highly significant with p<0.001. SPSS, version 17.0 was used in the analysis (SPSS Inc. Released 2008. SPSS Statics for Windows, version 17.0. Chicago: SPSS Inc.).
Results
The mean haemoglobin levels were lower in preeclampsia group as compared to standard pregnancy values [9]. Mean values of blood urea, S. creatinine and S. uric acid were higher in preeclamptic mothers as compared to standard reference values in pregnancy[9]. The mean age of mothers at time of delivery in group I and group II was 24.16 ± 1.86 years and 24.28 ± 2.15 years respectively. Mean gestational age of group I and group II were 37.52+0.59 weeks and 37.24+0.88 weeks. In majority of subjects (80% in group I and 58% in group II), gestational age at time of delivery was 36-41 weeks.
In the present study, majority of women had vaginal delivery in both the categories i.e. 100% in normotensive mothers and 72% in preeclamptic women. There were 3 preterm deliveries and 4 lower segment caesarean section (LSCS) in preeclamptic group and control group had no preterm delivery or LSCS (i.e. eighty four percent in normotensive deliveries (vacuum/forceps) in group II as compared to two percent in group I). Sixteen percent of preeclamptic had delivery by caesarean section. Forty percent of babies of preeclamptic mothers had 1 minute Apgar score <7 as compared to zero percent in normotensive mothers.
Majority of the babies had birth weight between 2.1-2.5 kg was 96% of normotensive pregnant women and 88% of preeclamptic women and rest of the babies were in the range of 2.6-3.0 kg. Mean birth weight in group I and group II was 2.34±0.19 kg and 2.29±0.18 kg respectively. Birth weight was lowered in pregnancy with preeclampsia as compared to normotensive women, but, it was not statistically significant (p>0.05).
In preeclamptic women HO-1 levels were higher in male babies as compared to female babies but it was not statistically significant (p>0.05). HO-1 levels were elevated in cord blood of female babies as compared to male babies of both normotensive pregnant and preeclamptic women, but, the difference was not statistically significant.
Discussion
Gender-based differences in the incidence of hypertensive and coronary artery disease, development of the atherosclerosis are known, relatively little is known about the effect of sex hormone on HO-1 activity.
In the present study, maternal HO-1 were higher in mothers with female babies as compared to male babies (285.30 ± 28.40 vs. 268.41 ± 35.00 ng/ml, p>0.05) in group I. Maternal HO-1 were higher in preeclamptic mothers with male babies as compared to female counterparts in group II (580 ± 111.28 vs. 526.2 ± 74.3 ng/ml, p>0.05). In the present study, umbilical cord blood HO-1 levels were higher in female babies as compared to male babies in group I (285.30 ± 28.40 vs. 268.41 ± 35.00 ng/ml, p>0.05). In group II cord blood HO-1 levels were higher in male babies as compared to female babies (580±111.28 vs. 526.94±73.98 ng/ml, p>0.05). However, no reports regarding gender based differences in cord blood HO-1 are available.
Gender differences in vascular and myocardial HO expression and activity are known. Several hypotheses have been postulated for the gender related difference of cardiovascular morbidity and mortality including differences in hormones, lipid profile, and myocardial, endothelial, and vascular performance between male and female gender and aging [10]. A great part of the observed gender differences in vascular reactivity has been attributed to genomic modulation by sex hormones, nongenomic effects of those hormones also exist [6].
Relatively little is known about the effect of sex hormones on HO activity during pregnancy. The AA genotype of HMOX-1 has been associated with an increased incidence of hypertension in women [10]. Ariyoshi et al. examined the effects of age and sex on microsomal heme oxygenase activity and cytochrome P-450 content in rat liver. They observed that heme oxygenase activity declined with an increase in age, namely, its activity in 100 days old (young) rats was 58% in male and 72% in female rats as compared with respective 30-day-old (immature) rats, and in 300-day-old (old) rats, and it was 32% in male and 39% in female rats [11].
The findings of high serum HO-1 levels in maternal and cord blood in preeclampsia in the present study supports the role of oxidative stress and excessive inflammatory response in the pathogenesis of preeclampsia. The present study revealed gender difference in normal and preeclamptic pregnancies and this may possibly contribute to the gender-difference of cardiac function and future risk of development of cardiovascular diseases. Several hypothesis have been postulated for the gender-related difference of cardiovascular morbidity and mortality including differences in hormones, lipid profile, and myocardial, endothelial and vascular performances between male and female genders and ageing [10].
The role of sex hormones in regulation of HO-1 has not been extensively studied. One study has observed the sex influences of hepatic expression of HO-1 following trauma and haemorrhage found that HO-1 expression and its activity were increased in females as compared to males [12]. Bonacasa et al. reported that female streptozocin-induced diabetic rats had higher HO-1 induction as compared to male rats [12,13]. Female Wistar rats had elevated cardiac levels of HO activity and expression, which may play a role in sexual dimorphism of cardiovascular ischemia-induced injury [14]. HO-1 levels were found to be significantly higher in the adipose tissue with polycystic ovary syndrome (PCOS) indicating the importance of HO-1 beneficial compensatory role in the adipose tissue of PCOS women [15].
While a great part of the observed gender differences in vascular reactivity has been attributed to genomic modulation by sex hormones, non-genomic effects of hormones also exist. Estrogen had generally been considered a protective factor against cardiovascular disease, which was based on epidemiological data showing that the incidence of coronary heart disease among women was lower than among men before menopause, a and this disparity decreased postmenopausal. It has been also seen that estrogen administration up regulates HO activity following traumatic injury and trauma haemorrhage [10-16].
Several studies had reported the important role of sex hormone in the regulation of blood pressure in male and females [16,17]. Peter et al. observed that adipose specific deletion of HO-1 resulted in increased fat mass, fasting hyperglycaemia and insulinemia in female mice fed both high and normal fat diets. These results suggest that adipocyte HO-1 plays a greater protective role in female versus males and strategies to preserve adipocyte HO-1 may have greater overall metabolic effects in females than males [18].
Although the mechanism by which estrogen affects vascular tone are not completely understood, and a change in the communication between the vascular endothelium and smooth muscle is likely important pathway for the action of estrogen. The mechanism by which gender influences CO production is unclear and may involve an increase in HO expression and activity.
Findings of changes in HO-1 enzyme system in a gender-dependent manner in the present study may be of help to explain the differences observed in cardiovascular disease risk between the sexes. Finding of higher values of HO-1 in maternal and cord blood of female babies as compared to male counterparts lends support to the potential beneficial effect of physiological estrogen. Cord blood levels of HO-1 remained higher in female babies of preeclamptic mothers as compared to male babies. However, preeclamptic mothers with male babies showed higher serum HO-1 levels as compared to female counterparts, suggesting that mothers of male babies might have increased risk of future cardiovascular events similar to the risk faced by adult males.
Demonstration of gender based changes in the present study supports the idea of active contribution of placenta to maternal metabolism during pregnancy. Also, results from the present study implicate HO-1 and possibly CO as important cardioprotective agents in the “female advantage” in cardiovascular function. This generates a new hypothesis on the possible role of oxidative stress, dyslipidemia and preeclampsia during pregnancy and future risk of cardiovascular disease.
REFERENCES
- Maryland B (2000) NHBPEP (National High Blood Pressure Education Programme) Report of National High Blood Pressure Education Programme Working Group In High Blood Pressure In Pregnancy. Am J Obstet Gynecol 183:1-22.
- Granger JP, Alenander BT, Llinas MT, Bennett WA, Khalis RA (2001) Pathophysiology of hypertension during preeclampsia linking placental ischemia with endothelial dysfunction. Hypertension 38:718-722.
- Soares MP, Marguti I, Cunha A, Larsen R (2009) Immunoregulatory effects of HO-1: how does it work? Curr Opin Pharmacol 9: 482-489.
- Zenclussen ML, Jensen F, Rebelo S, El-Mousleh T, Casalis PA, et al. (2010) Heme oxygenase-1 expression in the ovary dictates a proper oocyte ovulation, fertilization, and corpora lutea maintenance. Am J Reprod Immunol 67: 376- 382.
- Zenclussen ML,Casalis PA, El-Mousleh T, Rebelo S, Langwisch S, et al. (2011) Heme oxygenase-1 dictates intrauterine fetal survival in mice via carbon monoxide. J Pathol 225:293-304.
- Abraham NG, Kappas A (2008) Pharmacological and clinical aspects of heme oxygenase. Pharmacol Rev 60:79-127.
- Zenclussen ML, Casalis PA, Jensen F, Woidacki K, Zenclussen AC (2015) Hormonal fluctuations during the estrous cycle modulate heme oxygenase-1 expression in the uterus. Front Endocrinol 5: 32.
- Moniz CF, Nicolaides KH, Bamforth FJ, Rodeck CH (1985) Normal reference ranges for biochemical substances relating to renal, hepatic and bone function in fetal and maternal plasma throughout pregnancy. J Clin Path 38:468-472.
- Pósa A, Kupai K, Ménesi R, Szalai Z, Szabó R, et al. (2013) Sexual dimorphism of cardiovascular ischemia susceptibility is mediated by Heme Oxygenase-1. Oxid Med Cell Longev 2013:521-563. Epub
- Kharb S, Sardana D, Nanda (2012) Cord blood atherogenic index in preeclampsia: tracing fetal origins of adult disease. Res J Obstet Gynecol 5: 4-7
- Ariyoshi T, Tsuboi K, Hamasaki K (1981) Effects of age and sex on microsomal heme oxygenase and cytochrome P-450 content in liver of rats. J Pharmacobio-Dyn 4:664–669.
- Toth B, Yokoyama Y, Kuebler JF, Schwacha MG, Rue LW, et al. (2003) Sex differences in hepatic heme oxygenase expression and activity following trauma and hemmorhagic shock. Arch Surg 138: 1375-1382.
- Bonacas B, Prez C, Salom MG, Lopez B, Saez-Belmonte F, et al. (2013) Sexual dimorphism in renal heme-heme oxygenase system in the streptozocin diabetic rats. Curr Pharm Des 19: 2678-86.
- Posa A, Kupai K, Menesi R, Szalai Z, Szabo R, et al. (2013) Sexual dimorphism of cardiovascular ischemia susceptibility is mediated by heme oxygenase. Oxid Med Cell Longev
- Manneras-Holm L, Benrick A, Stener –Victorin E (2014) Gene expression in subcutaneous adipose tissue differs in women with polycystic vary syndrome and controls matched pair-wise for age, body weight, and body mass index. Adipocyte 3:190-196.
- Reckelhoff JF, Roman RJ (2011)Androgens and hypertension: Role in both males and female? Hypertension 57: 681-682.
- Maranon R, Reckelhoff JF (2013) Sex and gender differences in control of blood pressure. Clin Sci 125: 311-318.
- Horsick PA, Weeks MF, Hankins MW, Moore KH, Stec DE (2017) Sex-dependent effects HO-1 deletion from adipocyte in mice. Int J Mol Sci1 8: 611-613.